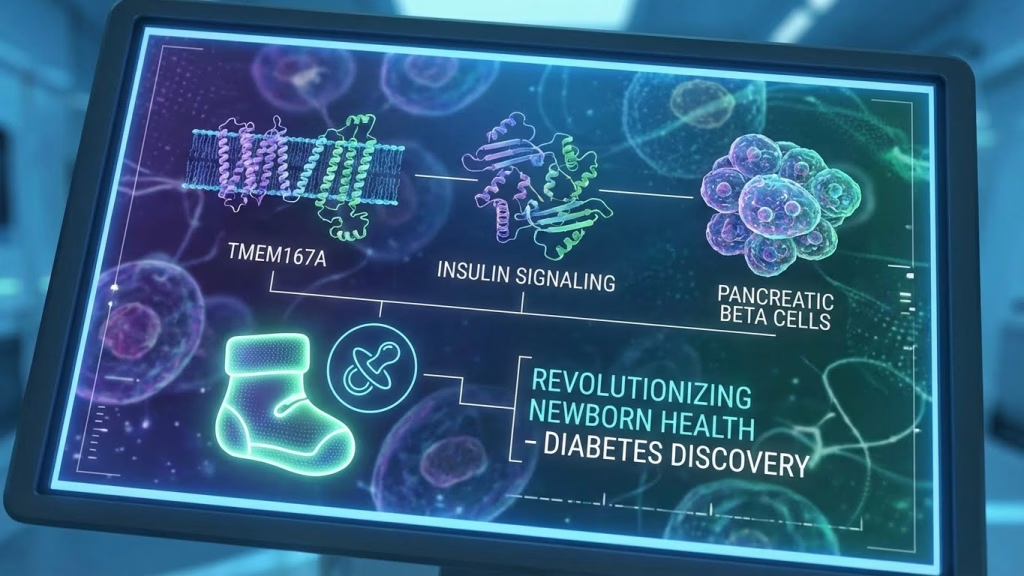
3 Explosive TMEM167A Genetic Diabetes Discoveries Revolutionizing Newborn Health
On This Page
Greetings, future shapers! Mason Rivers here, your guide through the gleaming spires of tomorrow’s tech. Today, we’re not just talking about gadgets or AI algorithms; we’re peering into the very blueprint of life itself, uncovering breakthroughs that promise to transform the earliest moments of human existence. Imagine a world where genetic predispositions are not sentences, but simply challenges swiftly overcome. That future is arriving, and nowhere is it more thrilling than in the fight against conditions like TMEM167A genetic diabetes. This challenging condition, once a daunting diagnosis for newborns, is on the cusp of being completely manageable, perhaps even preventable. We’re about to dive deep into three explosive discoveries redefining newborn health, particularly for those facing the challenges of TMEM167A genetic diabetes.
In a landscape increasingly defined by personalized medicine and proactive health, the advancements in understanding and treating TMEM167A genetic diabetes are nothing short of miraculous. We’re moving beyond reactive treatment to a visionary era of pre-emptive, precise intervention. Get ready to witness the dawn of an age where every child is given the healthiest possible start, fortified by the power of cutting-edge science and compassionate innovation.
The Dawn of Precision Genetics: Early Screening for TMEM167A Genetic Diabetes
The first revolutionary wave in tackling TMEM167A genetic diabetes arrives with unprecedented precision in early detection. Forget the days of late diagnoses and reactive treatment plans. Our current trajectory points to a reality where comprehensive prenatal and neonatal genetic screening becomes standard, powered by rapid, cost-effective whole-genome sequencing and advanced bioinformatics. Picture this: a newborn’s entire genetic code mapped within hours of birth, identifying specific markers for conditions like TMEM167A genetic diabetes long before symptoms even hint at an issue. AI-driven algorithms will analyze these vast datasets, not just flagging potential risks, but predicting the exact disease progression and potential therapeutic responses based on millions of anonymized genetic profiles.
This isn’t just about identification; it’s about immediate, personalized action. Upon detection of TMEM167A genetic diabetes, parents and medical teams will receive a tailored care pathway, informed by predictive analytics. This might include specific dietary recommendations, targeted monitoring protocols, or even the immediate initiation of precision therapies designed to mitigate the earliest cellular impacts. Imagine a future where a potential health crisis is averted before it truly begins, all thanks to a microscopic glimpse into a newborn’s unique genetic identity. This proactive approach to TMEM167A genetic diabetes is fundamentally changing the narrative from management to pre-emption.
Targeted Therapies and Gene Editing Breakthroughs
Our second monumental leap forward involves direct intervention at the genetic level. CRISPR-Cas9, once a sci-fi dream, is now evolving into a sophisticated toolkit capable of correcting the very errors that lead to conditions like TMEM167A genetic diabetes. Picture a future where, upon early detection, gene-editing therapies can be administered *in utero* or immediately post-birth, correcting the faulty TMEM167A gene responsible for the diabetes. These aren’t blunt instruments; next-generation editors are achieving unprecedented precision, minimizing off-target effects and offering a genuine chance for a functional cure rather than just symptom management.
Beyond permanent gene correction, pharmacogenomics is ushering in an era of hyper-personalized medication. For newborns diagnosed with TMEM167A genetic diabetes, drug formulations will no longer be one-size-fits-all. Instead, they will be custom-engineered based on the child’s individual genetic makeup, optimizing efficacy and virtually eliminating adverse reactions. Furthermore, advancements in regenerative medicine are showing incredible promise. Imagine stem cell therapies capable of regenerating or replacing the pancreatic beta cells damaged by TMEM167A genetic diabetes, effectively restoring the body’s natural insulin production mechanism. These therapeutic avenues represent a profound shift, offering hope for children to grow up free from the daily burden of this condition.
The Connected Nursery: Real-time Monitoring and Predictive AI for TMEM167A Genetic Diabetes
Our third groundbreaking discovery transforms the newborn’s environment into a sanctuary of continuous, intelligent care. The nursery of tomorrow will be a hyper-connected ecosystem, featuring advanced wearable technologies for infants. Think smart onesies or miniature, non-invasive patches that continuously monitor a baby’s glucose levels, heart rate, oxygen saturation, and even subtle metabolic markers. These devices will feed a constant stream of biometric data to sophisticated AI algorithms, which will learn each child’s unique physiological patterns.
This isn’t just about data collection; it’s about predictive action. For newborns with TMEM167A genetic diabetes, these AI systems will become vigilant guardians, capable of forecasting glycemic events – both highs and lows – hours before they manifest. Imagine an alert sent to parents and pediatricians, not just when a problem occurs, but *before* it has a chance to develop. Furthermore, these systems will integrate seamlessly with advanced closed-loop insulin delivery devices, evolving into fully adaptive bio-regulators that autonomously adjust insulin delivery based on predictive models, dietary input, and activity levels. The goal is to maintain perfect glycemic control, ensuring optimal brain development and growth without the constant vigilance that previously burdened families facing TMEM167A genetic diabetes.
This level of real-time monitoring and predictive intervention ensures that children with TMEM167A genetic diabetes can thrive, experiencing normal development unhindered by the unpredictable swings of blood sugar. It’s a testament to how human ingenuity, combined with machine intelligence, can create a truly protective environment for our most vulnerable.
Building a Holistic Ecosystem for Early Life Care
These individual breakthroughs coalesce into something even more powerful: a holistic, integrated ecosystem for early life care. The data gathered from precision screenings, ongoing genetic therapies, and real-time monitoring devices will all converge on secure, cloud-based platforms. These platforms will serve as central hubs for collaborative care, allowing parents, pediatricians, geneticists, and specialized dietitians to share insights and refine treatment plans in real-time. This interconnectedness ensures that every aspect of a child’s development, especially those managing TMEM167A genetic diabetes, is meticulously supported and optimized.
Moreover, this ecosystem extends beyond medical intervention. It informs personalized nutritional science, crafting bespoke dietary plans guided by a child’s unique genetic profile and metabolic needs. Imagine a scenario where a baby’s formula or early solid foods are precisely calibrated to their genetic propensity for TMEM167A genetic diabetes, preventing complications before they even arise. Access to these cutting-edge insights and technologies will become more democratized, too. Initiatives like the International Newborn Genomics Initiative are working to ensure that these life-saving advancements reach every corner of the globe, fostering health equity and giving every child a fighting chance.
Empowering Families and Future Generations
The profound impact of these discoveries extends far beyond the medical realm; they empower entire families. The anxiety and constant vigilance that once characterized parenting a child with TMEM167A genetic diabetes will be dramatically reduced. Parents will gain peace of mind, knowing that their child is receiving the most advanced, personalized care imaginable, supported by intelligent systems that proactively safeguard their health. This enables children born with TMEM167A genetic diabetes to experience a childhood free from the limitations and constant medical interventions that have historically been unavoidable.
We are talking about a future where a diagnosis of TMEM167A genetic diabetes is met with a robust, pre-designed pathway to normal development and thriving health. This isn’t merely about managing a condition; it’s about unlocking a child’s full potential, ensuring they can grow, learn, and play without the shadow of chronic illness. These advancements will pave the way for a generation of healthier, happier children, embodying the ultimate triumph of human innovation over adversity.