5 Shocking Auto-Brewery Syndrome Facts That Will Blow Your Mind
On This Page
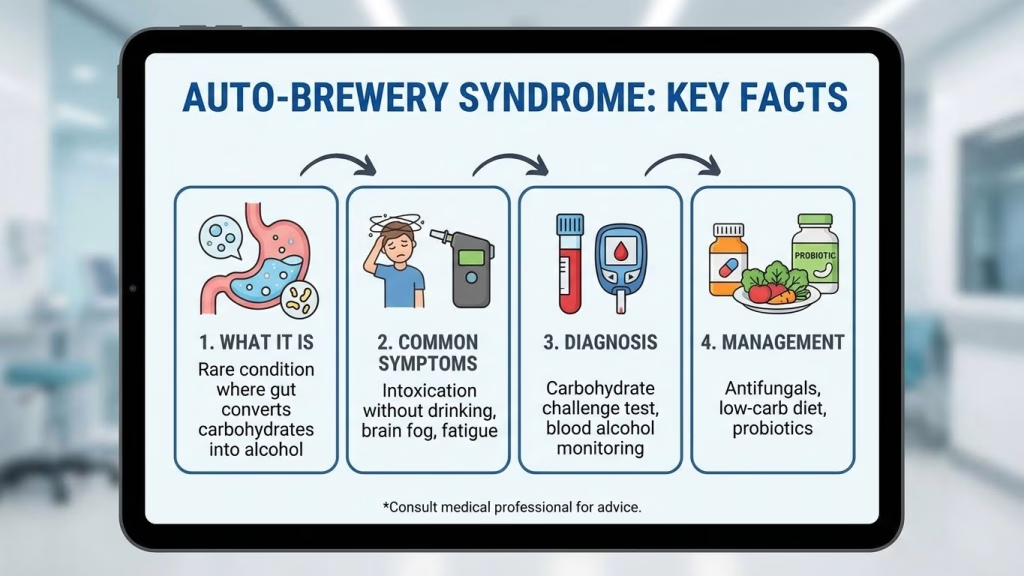
Imagine waking up feeling tipsy, experiencing all the symptoms of alcohol intoxication – dizziness, impaired coordination, even a hangover – yet you haven’t touched a single drop of alcohol. This isn’t a sci-fi premise; it’s the bewildering reality of Auto-Brewery Syndrome, a condition where your own gut bacteria produce alcohol. While rare, reported cases indicate a profound impact on individuals, with some exhibiting blood alcohol levels equivalent to several drinks, all without consuming anything externally. Today, we’re diving deep into five shocking facts about Auto-Brewery Syndrome that illustrate just how intricate and powerful our internal microbial ecosystems truly are.
It’s Not Just About Yeast in Auto-Brewery Syndrome
For many, the concept of internal alcohol production immediately conjures images of brewer’s yeast, Saccharomyces cerevisiae, fermenting sugars. While this fungus can indeed be a culprit in Auto-Brewery Syndrome, emerging research, particularly in the last decade, points to bacterial overgrowth as an equally significant, if not more prevalent, factor. Specifically, species like Klebsiella pneumoniae, a common gut resident, have been strongly implicated. Studies have shown elevated counts of these bacteria in ABS patients, capable of converting carbohydrates into ethanol through similar anaerobic fermentation pathways found in yeast. This revelation expands our understanding of the syndrome beyond fungal infections, highlighting the complex interplay of bacteria and fungi in the human gut and their potential to disrupt normal physiological functions.
Diagnosing This Baffling Condition Is a Nightmare
The clinical presentation of Auto-Brewery Syndrome often mirrors alcohol intoxication, leading to severe diagnostic challenges, skepticism from medical professionals, and immense personal distress for patients. Imagine trying to convince a doctor you’re sober while blowing a 0.08 BAC. Many patients suffer for years, misdiagnosed with psychiatric disorders, chronic fatigue, or even accused of secret alcoholism. A definitive diagnosis often requires specialized testing, such as a carbohydrate challenge. During this test, patients consume a measured dose of glucose, and their blood alcohol levels are monitored over several hours in a controlled environment, ensuring no external alcohol intake. This process alone can be lengthy and inconclusive, contributing to diagnostic delays that average several years for many patients, severely impacting their quality of life and mental well-being.
The Dietary Link and Its Profound Impact on Auto-Brewery Syndrome
For individuals grappling with Auto-Brewery Syndrome, diet isn’t just a preference; it’s a critical control factor. A diet high in refined carbohydrates and sugars provides the perfect substrate for the overgrowing yeast and bacteria in the gut to ferment, leading to elevated ethanol production. Think of your gut as a tiny, highly efficient brewery, and carbohydrates as the raw material. When the microbial balance is skewed towards alcohol-producing species, consuming a standard Western diet can become a constant source of internal intoxication. Clinical observations strongly suggest that strict adherence to low-carbohydrate diets can dramatically reduce symptom severity, in some cases bringing daily blood alcohol fluctuations to negligible levels. This direct correlation underscores the gut’s metabolic power and our food choices’ profound influence on our internal chemistry.
A Global Phenomenon, Not Just a Western Anomaly
While the earliest well-documented cases of Auto-Brewery Syndrome emerged from Japan in the 1970s, it’s a misconception to view it as a geographically limited or culturally specific condition. Reports of ABS are now recognized worldwide, with documented cases spanning North America, Europe, and Asia. Its perceived rarity might be more a function of underdiagnosis and lack of widespread medical awareness rather than actual prevalence. Factors like variations in dietary habits – such as high-starch diets common in certain cultures – or a history of significant antibiotic use impacting gut flora, could potentially influence the predisposition or manifestation of this condition in different populations. The global recognition of ABS highlights the universal susceptibility of the human gut microbiome to imbalances, regardless of geographical location. Further research suggests a broader distribution than previously assumed, emphasizing the need for global medical awareness.
Treatment Relies on Gut Ecosystem Manipulation
Treating Auto-Brewery Syndrome requires a holistic, multifaceted approach focused on restoring microbial balance. This often begins with rigorous dietary modifications, primarily a very low-carbohydrate, anti-fungal diet to starve the problematic microbes of their fuel source. Beyond diet, medical interventions can include targeted antifungal medications (e.g., nystatin, fluconazole) to combat yeast overgrowth, and sometimes specific antibiotics if bacterial species are identified as the primary culprits. However, antibiotic use is approached with caution to avoid further dysbiosis, which could exacerbate the problem. More advanced, albeit experimental, therapies like fecal microbiota transplantation (FMT) have shown significant promise in recalibrating the gut microbiome, essentially “resetting” the internal ecosystem and potentially eradicating the alcohol-producing organisms, offering a profound shift in patient recovery. The goal is to cultivate a healthy, diverse microbiome that can outcompete the “brewers.”
What Does Auto-Brewery Syndrome Teach Us About Our Internal Ecosystems?
The bizarre reality of Auto-Brewery Syndrome stands as a powerful testament to the profound influence our gut microbiome wields over our physiology. It illustrates how slight imbalances in microbial communities can manifest in systemic, debilitating ways, challenging our fundamental understanding of health and disease. As we delve deeper into the complexities of personalized medicine and the microbiome, conditions like ABS underscore the critical need for advanced diagnostic tools and targeted interventions. Understanding this internal brewery moves us closer to a future where gut health isn’t just about digestion, but about managing an entire internal chemical factory that shapes our very existence. The precision required to diagnose and treat ABS speaks volumes about the future of microbial therapeutics and our continuous journey to unlock the secrets within.