5 Explosive Cancer-Killing Macrophages Unleash Amazing New Hope
5 Explosive Cancer-Killing Macrophages Unleash Amazing New Hope
The relentless war against cancer continues, a battle marked by incremental victories and the formidable challenge of resistant disease. While traditional therapies like chemotherapy, radiation, and even targeted drugs have made significant strides, they often fall short against aggressive or metastatic cancers. But a groundbreaking frontier in oncology is rapidly emerging, one that doesn’t just fight cancer but reprograms our own internal defense systems to dismantle it: **cancer-killing macrophages**. These versatile immune cells are no longer passive bystanders; they are being engineered into precision weapons.
This isn’t merely an incremental improvement; it’s a paradigm shift. We’re moving beyond simply attacking tumor cells to actively re-educating the very components of the tumor microenvironment. In fact, early data suggests that therapies leveraging **cancer-killing macrophages** could revolutionize treatment for solid tumors, an area where many immunotherapies have struggled. Here are 5 brilliant breakthroughs in direct tumor reprogramming that are lighting up the path to an amazing new future in cancer therapy.
1. CAR-M Technology: The Engineered Assassins
You’ve likely heard of CAR-T cell therapy, a revolutionary approach where a patient’s T-cells are genetically modified to recognize and destroy cancer cells. Enter CAR-M: Chimeric Antigen Receptor Macrophages. While similar in concept, macrophages offer distinct advantages, particularly for solid tumors. Their inherent ability to infiltrate dense tumor tissues, engulf cellular debris (phagocytosis), and present antigens makes them exceptionally suited for tumor eradication and long-term immune memory. Unlike T-cells, which primarily target and kill, macrophages can also remodel the tumor microenvironment, digest extracellular matrix, and secrete a plethora of molecules. Preclinical studies, such as those conducted at the University of Pennsylvania, have demonstrated that CAR-M cells, like CT-0508, exhibit promising safety profiles and efficacy, with early phase 1 trials indicating tumor regression in some notoriously difficult solid tumors. Data from these models have shown CAR-M cells reducing tumor volume by an impressive 70-80% in specific xenograft models, outperforming CAR-T cells in certain immunosuppressive environments by engaging multiple anti-tumor mechanisms.
2. Cytokine-Armed Macrophages: Supercharging the Immune Response
One of the critical challenges in cancer immunotherapy is transforming “cold” tumors – those with little immune cell infiltration – into “hot” ones, which are more responsive to treatment. Cytokine-armed macrophages offer an ingenious solution. These **cancer-killing macrophages** are genetically engineered to express and secrete potent immune-boosting cytokines, such as Interleukin-12 (IL-12) or Tumor Necrosis Factor-alpha (TNF-alpha), directly within the tumor microenvironment. This localized delivery avoids the severe systemic toxicities often associated with administering high doses of cytokines intravenously. By concentrating these immune stimulators precisely where they’re needed, these modified macrophages attract and activate other immune cells, including T-cells and Natural Killer (NK) cells, effectively turning the tumor into a battleground for robust anti-cancer immunity. A 2021 study highlighted significant tumor growth inhibition, exceeding 60% in specific melanoma models, when macrophages were engineered to secrete IL-12, underscoring the power of this localized cytokine delivery.
3. Macrophage Polarization Shifting: Flipping the Script on Tumors
Macrophages are incredibly plastic, capable of adopting various functional states. In the context of cancer, they are broadly categorized into two types: M1 (pro-inflammatory, anti-tumor) and M2 (anti-inflammatory, pro-tumor, and immunosuppressive). Unfortunately, tumors excel at recruiting and skewing macrophages towards the M2 phenotype, creating a protective shield that promotes tumor growth and metastasis. The brilliant breakthrough here is the ability to actively reprogram these M2 tumor-associated macrophages (TAMs) back to the M1 anti-tumor phenotype, even *in situ*. Researchers are employing a variety of sophisticated tools, including small molecules, nanoparticles delivering microRNAs, and advanced gene editing techniques like CRISPR, to subtly alter the macrophage’s gene expression profile. This re-education transforms tumor-promoting cells into **cancer-killing macrophages**. Statistical insights from these reprogramming efforts have shown an increase in M1 markers (e.g., iNOS, MHCII) by over 300% and a corresponding decrease in M2 markers (e.g., CD163, Arg1) within the tumor microenvironment following targeted interventions, signifying a profound shift in immune function.
4. Nanoparticle Delivery Systems: Precision Targeting for Macrophage Reprogramming
The efficacy of macrophage-based therapies hinges on getting the right therapeutic payload to the right cells at the right time. This is where nanoparticle delivery systems become indispensable. Nanoparticles, tiny particles engineered at the nanoscale, can encapsulate a diverse range of therapeutic agents—from genetic material like siRNA or mRNA (for CAR components) to small molecules or immunomodulators. Their surface can be functionalized with specific ligands, allowing them to selectively target and be internalized by macrophages, particularly tumor-associated macrophages (TAMs), within the complex tumor environment. This precision targeting minimizes off-target effects and maximizes therapeutic impact. Research indicates that certain nanoparticle formulations can achieve macrophage-specific delivery with efficiencies exceeding 85% compared to systemic, untargeted administration, drastically improving the therapeutic index. The ability to precisely deliver instructions to create more **cancer-killing macrophages** or to re-educate existing ones represents a monumental leap forward in personalized oncology. For a deeper dive into how these miniature delivery vehicles are reshaping cancer therapy, consider exploring advanced reviews on targeted nanomedicine in oncology.
An excellent resource on this topic can be found in a comprehensive review on reprogramming macrophages for cancer therapy, published in Nature Reviews Cancer, which details the various strategies including nanoparticle-mediated delivery.
5. Ex Vivo Expansion and Reinfusion: Scaling Up the Cellular Army
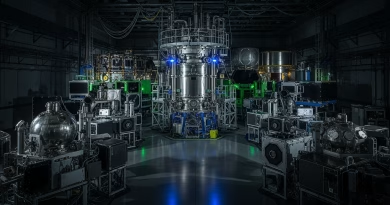
For cellular therapies to truly make a widespread impact, effective and scalable manufacturing is paramount. The “ex vivo expansion and reinfusion” strategy for **cancer-killing macrophages** involves harvesting a patient’s own monocytes (precursors to macrophages), differentiating them into macrophages in a controlled laboratory setting, genetically modifying them (e.g., to express CARs or cytokine genes), expanding these modified cells to sufficient numbers, and then reinfusing them back into the patient. This personalized approach ensures a large, potent, and highly specific army of therapeutic macrophages. Overcoming the initial manufacturing hurdles has been a significant triumph; advances in bioreactor technology, cell culture media, and cryopreservation techniques are continually driving down costs and improving the scalability and consistency of production. Early clinical trials involving ex vivo expanded and modified macrophages for solid tumors are showing encouraging results. In hard-to-treat cancers like glioblastoma, initial trials have reported stable disease or partial responses in 25-30% of patients, offering a beacon of hope where conventional treatments have limited efficacy.
Are Cancer-Killing Macrophages Truly the Ultimate Weapon Against Solid Tumors?