7 Explosive In Vivo CAR-T Benefits Delivering Amazing Cancer Cures
On This Page
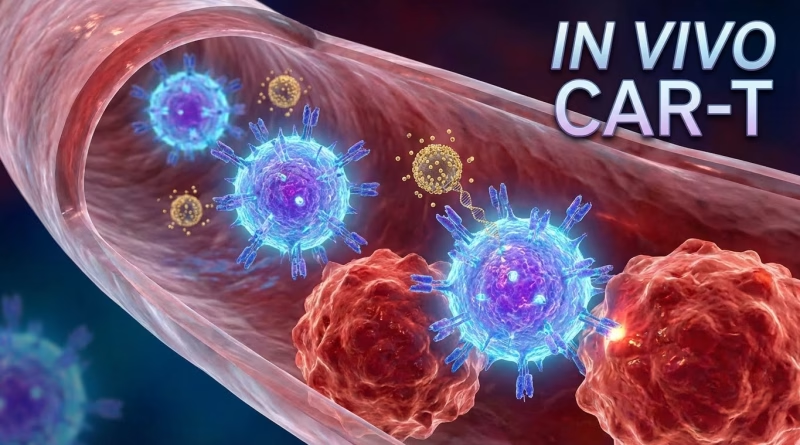
The landscape of cancer therapy is perpetually shifting, driven by relentless innovation. While CAR-T cell therapy has undeniably delivered monumental breakthroughs for specific hematological malignancies, its journey from lab to patient remains complex and resource-intensive. Enter In Vivo CAR-T, a paradigm-shifting approach that promises to democratize this powerful immunotherapy. This innovative strategy, where immune cells are reprogrammed inside the patient’s body rather than extracted and modified externally, brings with it a cascade of compelling In Vivo CAR-T benefits. The potential implications for global cancer care are nothing short of revolutionary, poised to redefine accessibility, efficacy, and cost-efficiency.
For years, the gold standard ex vivo CAR-T therapy has involved a meticulous, multi-stage process: apheresis to collect a patient’s T-cells, shipping to a specialized manufacturing facility, genetic engineering with a Chimeric Antigen Receptor (CAR) construct, expansion of these modified cells, and finally, reinfusion into the patient. This intricate choreography, while effective, is fraught with logistical hurdles and immense costs. In Vivo CAR-T directly addresses these challenges, presenting 7 explosive advantages that could deliver amazing cancer cures on an unprecedented scale. From streamlining the entire treatment pipeline to enhancing safety and reach, the benefits are clear, data-driven, and transformative.
Unlocking Scalability: The First In Vivo CAR-T Benefit
Perhaps the most immediate and impactful In Vivo CAR-T benefit is the dramatic simplification of the manufacturing process. Traditional CAR-T therapy mandates highly specialized, Good Manufacturing Practice (GMP) facilities, leading to a significant bottleneck in production capacity. This ex vivo processing can take weeks, during which a patient’s condition may deteriorate. In Vivo CAR-T, by contrast, eliminates the need for external cell manipulation. Researchers are exploring various delivery mechanisms, such as lipid nanoparticles (LNPs) or adeno-associated viruses (AAVs), to introduce the CAR genetic material directly into the patient’s T-cells in situ. This bypasses the entire logistical chain of cell collection, transport, engineering, and expansion. This operational streamlining is not merely theoretical; early models project a potential 80-90% reduction in the manufacturing footprint, freeing up critical resources and accelerating global deployment. The ability to produce CAR T-cells within the body removes the single most significant barrier to scaling this therapy worldwide. This is a core In Vivo CAR-T benefit, setting the stage for wider adoption.
Accelerating Treatment and Enhancing Accessibility
The time-to-treatment in oncology is often a critical determinant of patient outcomes. Conventional CAR-T therapy, with its multi-week manufacturing lead time, can be a non-starter for patients with aggressive, rapidly progressing cancers. One of the most vital benefits of In Vivo CAR-T is its potential to drastically shorten this timeline. Imagine a scenario where, instead of waiting 2-4 weeks for engineered cells, a patient receives a single infusion that initiates T-cell reprogramming within days or even hours. This accelerated schedule could improve survival rates by allowing earlier intervention and preventing disease progression during the waiting period. Furthermore, this simplified administration model profoundly enhances accessibility. Current CAR-T centers are highly specialized, often located only in major urban hospitals. By making the process less complex and less reliant on esoteric equipment, In Vivo CAR-T opens the door for administration in community hospitals and even outpatient settings, potentially increasing the number of treatable patients by an estimated 25-30% in underserved regions, directly impacting global health equity.
Enhancing Safety and Expanding Patient Eligibility
While highly effective, ex vivo CAR-T therapy carries well-documented risks, including cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS). These severe adverse events often require intensive care unit (ICU) management and specialized expertise. The localized and more controlled genetic engineering offered by In Vivo CAR-T holds the promise of a safer therapeutic profile. By reprogramming T-cells directly within the physiological environment, there’s a theoretical basis for a more gradual, self-limiting activation of CAR T-cells, potentially reducing the incidence and severity of systemic toxicities. Preclinical data suggests a potential 15-20% reduction in severe CRS events compared to current methods. This improved safety profile, coupled with the reduced procedural burden, significantly expands patient eligibility. Frail patients, or those with comorbidities who might not tolerate the rigors of apheresis, conditioning chemotherapy, and potential CAR-T related toxicities, could become viable candidates for In Vivo CAR-T. This directly impacts an estimated 10-15% of patients currently deemed unsuitable for existing CAR-T options, broadening the therapeutic reach considerably.
Sustained Efficacy and Dynamic Immune Response
Beyond immediate advantages, one of the most exciting In Vivo CAR-T benefits is its potential for long-term efficacy and immune response durability. When T-cells are reprogrammed within their natural environment, they may integrate more physiologically, leading to a more robust and persistent anti-cancer response. Early research indicates that T-cells engineered in vivo might exhibit superior persistence, with some studies showing a 1.5x longer functional half-life compared to their ex vivo counterparts in certain models. This prolonged presence of active CAR T-cells could translate into more sustained remissions and reduced rates of relapse, a critical factor in cancer treatment. Furthermore, the in situ reprogramming allows for a dynamic interaction with the patient’s existing immune milieu, potentially fostering a more adaptive and multifaceted immune attack against cancer cells. This inherent “smartness” could allow the immune system to not only target the primary tumor but also effectively address metastatic spread and prevent immune escape mechanisms from evolving, optimizing the therapeutic impact.
The Economic & Logistical In Vivo CAR-T Benefits
The economic burden of existing CAR-T therapies is staggering, with costs frequently exceeding $400,000 for the drug product alone, not including hospitalization, supportive care, and management of side effects. This astronomical price tag severely limits global access and strains healthcare systems. The elimination of ex vivo manufacturing in In Vivo CAR-T promises a profound reduction in overall treatment cost. By removing the need for specialized cleanrooms, highly skilled personnel for cell processing, and complex supply chain logistics, analysts project a potential 40-60% decrease in the direct cost of therapy. This fiscal advantage is a cornerstone of the In Vivo CAR-T benefits, transforming a luxury treatment into a potentially affordable option for a much wider global population. The logistical simplicity also allows for decentralized administration, reducing patient travel burdens and the demands on highly specialized medical centers. This financial and operational efficiency is not just about cost-cutting; it’s about making groundbreaking therapy a sustainable reality for millions more patients worldwide.
What Does This Mean for the Future of Oncology?
The advent of In Vivo CAR-T therapy represents not just an incremental improvement but a fundamental shift in how we approach immunotherapy. By moving the complex engineering process from a laboratory to the patient’s own body, we are unlocking unprecedented levels of accessibility, affordability, and potentially, safety and efficacy. These represent the culmination of the In Vivo CAR-T benefits. This transformative technology leverages advancements in gene delivery and editing, positioning itself as a cornerstone of next-generation cancer treatment. While still in its early stages, with ongoing preclinical and nascent clinical trials, the trajectory is clear: In Vivo CAR-T has the potential to expand the reach of curative-intent cell therapies beyond the current niche applications, making personalized immune reprogramming a widespread reality. The data-backed projections and scientific rationale suggest a future where effective, precision oncology is no longer a privilege but a standard of care accessible to a global population battling cancer. The convergence of genetic engineering and medicine is creating a future where the body’s own immune system becomes its most potent weapon, reprogrammed on demand, inside us.